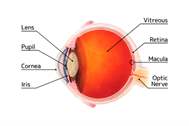
Keratoconus is a corneal disease generally characterized by frequently asymmetrical, noninflammatory corneal lesions, corneal thinning and corneal protrusion. Since it is noninflammatory it does not cause inflammation or vascularization in the cornea. Keratoconus is made up of the words cornea (kerato) and apex (conus) which are Greek. This structural defect of the cornea results in irregular astigmatism and myopia leading to impairment of visual quality. The beginning of keratoconus is gradual and generally the symptoms occur at early ages. Generally it starts at the age of 15-17.
Since its course is bilateral yet asymmetrical (one eye is affected more) it may occur in only one eye in the elementary cases. The disease typically progresses for years and then it is stabilized. Though keratoconus generally stops at the age of 30 or 40, it may start, progress or stop at any age. As the visual impairment may be corrected with glasses of soft lenses, most of the patients need hard, gas-permeable contact lenses in to reach a sufficient visual level. The disease keeps progressing in the 20% of the patients resulting in corneal transplant.
Frequency
The fact that keratoconus starts gradually and that the insignificant cases are generally not diagnosed complicate the estimation of the real frequency. As the frequency of keratoconus changes as per the regions, the most accurate data are available in the United States and the estimated frequency is 54.5 in 100.000 people. It means that 54.5 of a healthy population of 100.000 develop keratoconus.
This rate changes up to 230 in 100.000.
In a study, keratoconus was reported to be observed more in men. It was shown to occur mostly at the age of 15-24 in men as 25-34 in women. However, keratoconus is more frequently observed in the geographic area embodying Middle East and Turkey. The accompanying allergic eye diseases are observed more frequently within this geographic ares.
Risk Factors
Genetics and micro traumas are considered as responsible (Table 1 and 2). Also, it was reported that the enzymes that cause inflammation and tissue damage within the cornea are observed more in these patients and that the protective enzymes preventing the effect of these are less or none.
It has been shown that damaging radicals are increased by the sun light or rubbing the eyes.
It is known that the habit of rubbing the eyes is frequently seen in patients with keratoconus.
Keratoconus is more frequently observed in atopic patients (a concept relating to diseases such as hay rum, asthma, urticaria and eczema). Chronic eye rubbing has been found associated with keratoconus resulting in the inflammation of the disease. Especially, rubbing the eyes frequently during childhood should be realized by the parents and the eyes should be examined by the doctors in terms of allergic eye disease and hay rum. Prompt precautions prevent the development of keratoconus or its inflammation. Concurrence with certain systemic diseases has been reported.
The positive family history was reported as 6-23%. Actually, the fact that the insignificant cases are mostly not diagnosed among the members of the family, shows that the frequency of genetic is insufficient. I believe that the family factor is more dominating. Therefore, in case keratoconus is diagnosed the other members of the family should be examined for keratoconus.
Table 1. Risk Factors
Contact lens
Eye rubbing
Atopia
Leber congenital amaurosis
Ballon Mitral Valve
Positive Family History
Table 2.
Eye rubbing : Normal%58 Keratoconus%80
Positive Family History : Normal%0.05 Keratoconus%10
Symptoms
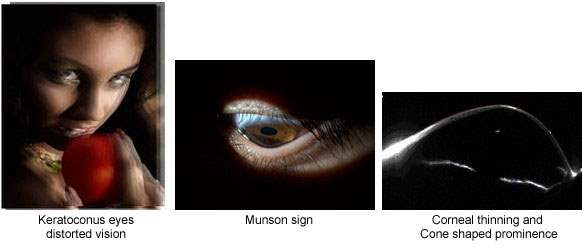
The symptoms are various and depend on the degree of the disease. Most of the time, there are no symptoms at the elementary phases. The diagnose occurs during the topography of the cornea or while investigating the reasons of fluctuations of diopter values, the inconvenient diopter values of the patients, visual impairment and headache in these periods. An evident visual irregularity and deep visual loss are seen in advanced cases.
Yet, complete blindness is never developed. Generally, no symptoms are observed in insignificant keratoconus cases. The ophthalmologist may observe the following corneal indications in moderate and advanced keratoconus cases.
Cone shaped prominence
This profile is easily realized with biomicroscope or with naked eye when the patient looks downward (Munson sign) in the cases of advanced keratoconus.
Thinning
Iron deposition
Vogt lines (Vertical lines in deep cornea)
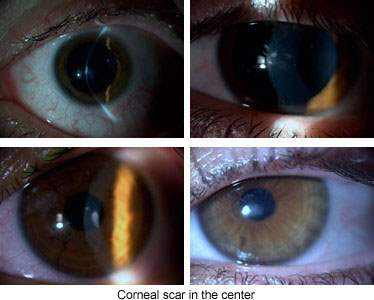
Scarring (Apical scar)
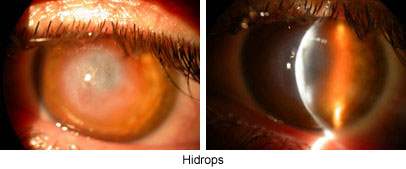
Sometimes extreme erection and thinning may result in cracking in the deep layers of cornea and penetration of the intraocular liquid into cornea leading to the formation of swollen and blurred cornea as a result of edema (Hidrops, see figure). Edema may last for weeks or months disappearing replaced by scars. Corneal hidrops does not develop any indications for keratoplasty; even the scar facilitates the usage of contact lenses by smoothing the cornea.
 Diagnose
Diagnose
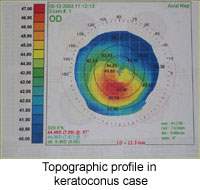
The diagnose is presented easily with topography (corneal map) even at the earliest periods.
Distinctive Diagnosis
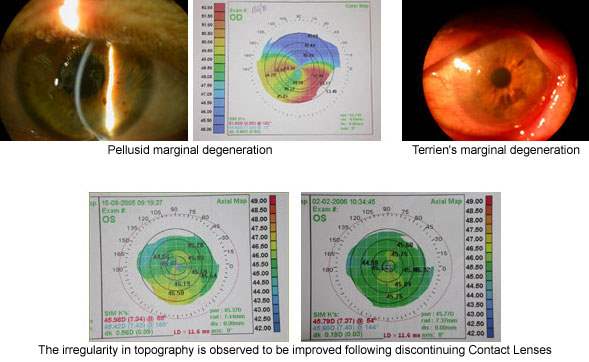
Keratoconus should be differentiated the other eclectic diseases of cornea standing out with thinning. As distinct the others, corneal thinning and erection is principal in keratoconus.
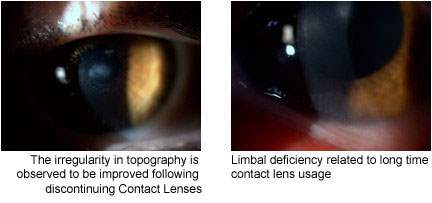
These are pellucid marginal degeneration, Terrien marginal degeneration and keratoglobus. Sometimes keratoconus may be mistaken for irregularities that occur in the cornea depending on contact lens usage (Contact lens warpage).
Treatment
The treatment changes depending on the degree of the disease. First of all underlying visual impairments that may result in micro traumas and eye rubbing should be treated such as allergic conjunctivitis and dry eye. The patients should be prevented rubbing their eyes. Allergic eyes reduce the tolerance of the lens.
Hard contact lenses are the basic steps of the treatment. Even if glasses are sufficient for the correction of visual impairment at the very early stages, hard contact lenses are required for the correction of irregular astigmatism that arises depending on the advancement of the disease. Generally, most of the patients benefit hard contact lenses. Yet, the adjustment of contact lenses is complicated for keratoconus. Generally, the patients get used to hard contact lenses in progress of time.
Serious complications are few related to hard lenses. The problems are corneal abrasion, apical scar (scar in the center of cornea), vascularization, discomfort depending on the contact lens and the instability of the lens over the cornea. The proper adjustment of contact lenses is important; otherwise corneal damage and advancement of keratoconus may be seen.
 Türkçe
Türkçe English
English
 German
German
 Spanish
Spanish